Definition
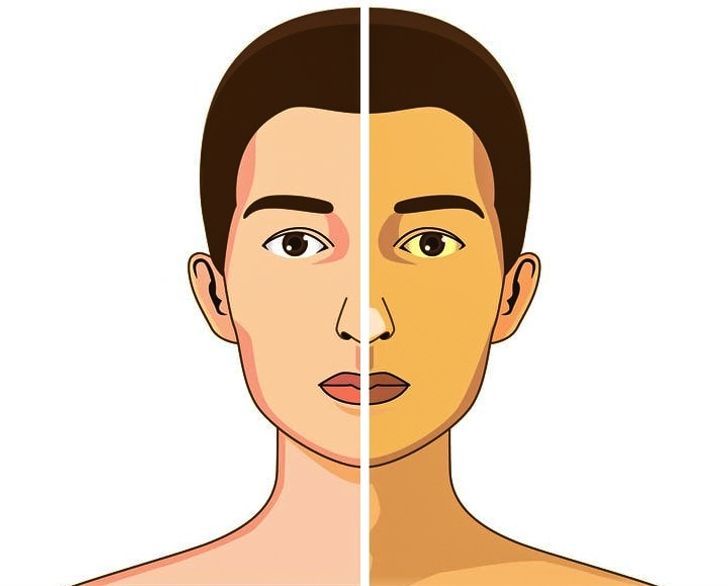
Jaundice is a condition in which the skin and mucous membranes are colored in different shades of yellow. Moreover, not in all cases this indicates pathological processes in the body.
Types of jaundice
Distinguish between false and true jaundice. False jaundice occurs when carotenes accumulate in the skin due to excessive consumption of carrots, beets, oranges, pumpkin, when ingested certain drugs (acriquine, picric acid, etc.).
True jaundice is a consequence of an increase in the concentration of total bilirubin in the blood plasma.
Icteric skin coloration and icterus (yellow pigmentation) of the sclera occur when the concentration of total bilirubin in the blood plasma is more than 35-45 μmol / l. Milk of lactating women, pleural and pericardial effusion, ascitic fluid, semen can have a yellow tint.
The clinical picture and duration of true jaundice depend on the underlying disease, against the background of which an increase in blood bilirubin developed.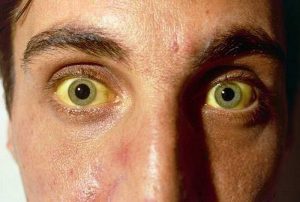
Distinguish:
1. Hemolytic (suprahepatic) jaundice:
jaundice due to genetic diseases (hereditary microspherocytosis, hereditary stomacytosis, etc.);
autoimmune (acquired) hemolytic anemia.
2. Parenchymal (hepatic) jaundice:
caused by infectious diseases (viral hepatitis A, B, C, D, E; herpetic hepatitis, cytomegalovirus hepatitis, yellow fever, infectious mononucleosis, relapsing fever, intestinal yersiniosis, psittacosis, leptospirosis, salmonellosis, pseudotuberculosis);
caused by non-infectious diseases (acute alcoholic hepatitis, drug hepatitis, liver cirrhosis, poisoning with oxidants based on nitric acid, hydrazine and its derivatives, chloroethane, ethylene glycol).
3. Constitutional jaundice (Gilbert’s syndrome, Crigler-Nayyard syndrome, Dabin-Johnson syndrome, Rotor syndrome).
4. Mechanical (subhepatic) jaundice occurs against the background of cholelithiasis, cholangitis, cicatricial strictures of the extrahepatic bile ducts, cancer of the pancreatic head, large duodenal papilla, gallbladder.
Hemolytic jaundice is characterized by mild manifestations, lemon staining of the skin, sclera, and mucous membranes, a slight enlargement of the liver, and often a markedly enlarged spleen. There is anemia.
In acute viral hepatitis, dull aching pains in the right hypochondrium and in the joints disturb, the temperature rises, the appetite decreases, the patient experiences weakness. Yellowness of the skin, dark urine and insufficiently colored feces appear. The skin may be bruised as a result of hemorrhages. Pruritus is not typical for acute viral hepatitis, since sufficient evacuation of bile through the bile ducts is ensured. When interviewing a patient, it is possible to identify a risk factor for the development of the disease (contact with patients with hepatitis, recent surgery, blood transfusions, injections and manipulations associated with a violation of the skin and mucous membranes).
With obstructive jaundice, the clinical picture may begin acutely or develop gradually.
With an acute onset of the disease (cholelithiasis), colicky pain suddenly appears in the right hypochondrium with irradiation to the right and to the back, chills, fever. Then jaundice and pruritus join. With the gradual development of the disease (cancer of the head of the pancreas), the patient may be disturbed by moderate dull or pressing pains under the right costal arch, nausea, belching, and weight loss. On palpation of the abdomen, pain in the right hypochondrium is determined. The yellowness of the skin gradually increases, the urine becomes dark in color, the feces become lighter, since less bilirubin is secreted into the intestines.
Constitutional jaundice is characterized by moderate intermittent (periodic) jaundice. Selective staining of the skin of the face, nasolabial triangle, palms, soles and axillary fossa is noted. Jaundice occurs or worsens after physical or mental stress, exacerbation of a concomitant disease, alcohol intake. The liver and spleen do not increase in size.
As a result of prolonged toxic effects of high concentrations of bilirubin on the body, damage to the central nervous system develops, foci of necrosis are formed in the parenchymal organs, the cellular immune response is suppressed, and anemia occurs. Children can have serious complications: nuclear jaundice, mental retardation, cerebral palsy.
Possible causes of jaundice
True jaundice is the result of an imbalance between the production and release of bilirubin. The cause of such a violation can be an increased formation of bilirubin (hemolytic jaundice), a failure in its transportation to liver cells and excretion by these cells, as well as a deterioration in the binding of free bilirubin (parenchymal jaundice). Obstructive jaundice is the result of a deterioration in the release of bilirubin through the extrahepatic ducts.
The mechanism of development of hemolytic jaundice is based on hemolysis (increased destruction of erythrocytes), when the life span of erythrocytes is significantly shortened, sometimes to several hours. Hemolysis can be intravascular and extravascular. Intravascular hemolysis occurs as a result of mechanical destruction of erythrocytes in small blood vessels (marching hemoglobinuria), turbulent blood flow with dysfunction of prosthetic heart valves, as a result of incompatibility of erythrocytes in the AV (0) system, rhesus or some other system, due to direct toxic effects ( snake venom), etc.
Extravascular hemolysis occurs in the spleen and liver as a result of the capture and destruction of altered red blood cells. The spleen is capable of capturing and destroying little-altered erythrocytes, the liver – erythrocytes with large disorders.
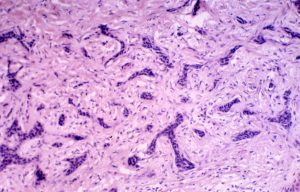
Hepatic (parenchymal) jaundice is mainly caused by damage to hepatocytes (liver cells). In some cases, this syndrome is associated with damage to liver cells and bile congestion, for example, in acute and chronic viral hepatitis. In others, the release of bilirubin is disturbed (with cholestatic jaundice, cholestatic hepatitis, primary biliary cirrhosis).
In case of violations of the outflow of bile through the extrahepatic bile ducts, obstructive (mechanical) jaundice occurs.
As a result of genetic defects in liver enzymes, enzymopathic or constitutional jaundice occurs. The most common is Gilbert’s syndrome, which develops against the background of a violation of the capture of free bilirubin and its binding to glucuronic acid due to a deficiency of the enzyme glucuronyl transferase.
In 60-80% of newborns, yellowness of the skin is observed, which appears on the 2-3rd day of life.
Jaundice of newborns can be caused by a high erythrocyte release during labor, a high content of fetal hemoglobin, rapid destruction of bilirubin after childbirth, and a deficiency of conjugating enzymes in the liver. At the same time, the rise in the level of bilirubin does not reach critical values, and the child’s condition remains satisfactory.
Breast milk jaundice (jaundice from breast milk) is not considered a pathology and is associated with the baby’s reaction to fats in breast milk. This condition develops on the 3-7th day after birth, when the child already receives a sufficient amount of mother’s milk. Stopping breastfeeding for 24-48 hours leads to a sharp decrease in bilirubin and a decrease in the severity of jaundice. If the child continues to receive breast milk, jaundice persists for 4-6 weeks, then gradually decreases – the condition of the skin and mucous membranes is normalized by the 12-16th week of life.
Hemolytic disease of newborns is caused by the incompatibility of the blood of the mother and the fetus for various antigens, when the body of a pregnant woman produces antibodies that penetrate the placental barrier into the blood of the fetus and cause destruction (hemolysis) of its erythrocytes. The intensity of jaundice depends on the level of bilirubin – when critical numbers are reached, this enzyme can affect the neurons of the brain, resulting in bilirubin encephalopathy (kernicterus).
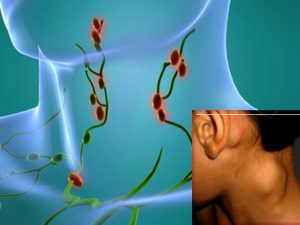
Which doctors to contact
When jaundice appears, to clarify the diagnosis and determine further treatment tactics, the patient must consult a general practitioner, therapist or pediatrician, if the patient is a child. In the future, consultation of a gastroenterologist, hematologist, oncologist, infectious disease specialist, surgeon may be indicated.
What to do with jaundice
Diagnosis and treatment of jaundice depends on the cause. Untimely prescribed therapy or self-medication may be ineffective, aggravate the course of the disease, and lead to complications. Therefore, it is important to consult a doctor, conduct an examination in full and follow all the recommendations of a specialist.
Jaundice treatment
The goals of jaundice therapy are reduced to the treatment of the underlying disease, which led to yellowness of the skin and mucous membranes, to improve the general condition of the patient, and to treat complications.
Conservative therapy may include:
a diet restricting fatty, smoked, spicy, spicy foods, pastry;
refusal from alcohol;
enzyme therapy (pancreatin, creon, festal, etc.);
antibiotic therapy;
antispasmodics;
blockers of gastric secretion;
infusion therapy;
correction of hemostasis disorders;
drugs that accelerate the exchange and excretion of bilirubin (barbiturates);
glucocorticosteroids;
vitamin therapy;
hepatoprotectors;
substances that bind bile acids in the intestine and reduce itching;
phototherapy.
According to the indications, the body is detoxified with the help of plasmapheresis.
Surgical treatment is most often required for obstructive jaundice https://en.wikipedia.org/wiki/Jaundice (tumor lesions of the liver, bile ducts, pancreatic head; stenosing strictures and stones of the biliary tract). The following surgical interventions can be performed:
endoscopic (through the natural openings of a person using endoscopic equipment);
laparoscopic (through small punctures using a laparoscope);
open method (by incision of the anterior abdominal wall).
If the treatment is ineffective, liver transplantation may be indicated.
In order to prevent jaundice, it is necessary:
prevent diseases leading to an increase in bilirubin;
carry out timely diagnosis and treatment of identified diseases;
follow all the doctor’s recommendations for liver pathologies;
give up alcohol.