Definition
Streptoderma (impetigo) is an infectious skin disease that is more common in childhood. It belongs to the group of pyoderma, which are based on purulent lesions of the skin, its appendages, as well as subcutaneous adipose tissue.
Reasons for the appearance of streptoderma
As the name of the disease suggests, streptococci are usually the causative agents of streptoderma.
Exogenous factors contributing to the development of the inflammatory process and its recurrence include:
violation of the integrity of the epidermis (microtrauma, skin maceration);
In adult patients, the infection can get into the skin as a result of non-observance of the rules of asepsis and antiseptics when performing cosmetic procedures (mesotherapy, peeling, etc.) or when using contaminated cosmetic instruments.
increased sweating (hyperhidrosis);
shift of skin pH to the alkaline side, the effect of high and low temperatures;
contamination of the skin.
Endogenous risk factors include:
various endocrinopathies (for example, diabetes mellitus);
insufficient intake of proteins into the body;
the presence of severe somatic diseases;
chronic intoxication;
the presence of foci of infection in various organs and tissues.
Streptoderma refers to an infectious disease and can be transmitted by contact (through a handshake, contact with a surface on which streptococcal infection is present, etc.) and airborne droplets.
Classification of streptoderma
Streptoderma can be superficial and deep.
Superficial streptoderma:
streptococcal impetigo,
slit impetigo,
paronychia,
papulo-erosive streptoderma,
intertriginous streptoderma,
erysipelas,
streptococcal toxic shock syndrome (STSS),
acute diffuse streptoderma.
Deep streptoderma:
cellulite,
ecthyma is vulgar.
There are three stages of streptoderma:
initial, when there are small purulent eruptions that resemble vesicles;
non-bullous, which develops after the opening of the vesicles and is characterized by the formation of streptococcal ecthyma (ulcerative streptoderma);
chronic, which develops either with improper therapy of the disease, or as a result of a decrease in immunity and is characterized by regular rashes.
Streptoderma symptoms
Streptococcal impetigo is observed in children of different age groups. It is characterized by the formation of flikten (elements of a rash) with serous or serous-purulent contents mainly on the skin of the face. As a result of the opening of the bubbles, ulcers are formed, which are covered with dry crusts, which fall off after 3-4 days. Scars after the disease are extremely rare.
For bullous impetigo, rashes with serous-purulent contents and surrounded by a pink corolla are characteristic. After opening, erosions are formed in their place, covered with a thin crust. Rashes are localized mainly on the lower extremities and the back of the hands.
Slotted impetigo (seizure) is a shallow crack, erosion, with a tendency to maceration (weeping). It is localized in the corners of the mouth, at the outer corners of the eyes, at the base of the wings of the nose.
Paronychia (superficial panaritium) is a flickenu on an inflamed base, localized around the nail plate.
Papulo-erosive streptoderma is observed in infants and is localized on the skin of the buttocks, the back and inner thighs, in the perineum, and the scrotum. The disease is characterized by dense cyanotic-red papules surrounded by inflamed skin. On the surface of the papules, conflicts form, which quickly open up with the formation of erosions and crusts.
Intertriginous streptoderma is localized on the contacting surfaces of large folds (inguinal, axillary, cervical, gluteal, behind the auricles). The bubbles quickly break open with the formation of weeping erosions, which have clear boundaries. This form of streptoderma is often found in children and adults with overweight, diabetes mellitus, and hyperhidrosis.
Erysipelas, as a rule, is localized on the legs, arms, trunk (in the places of surgical wounds), on the face (as a complication of rhinitis or conjunctivitis), in children – on the cheeks, in the periorbital region, on the neck and limbs. Inflammation is represented by erythema with raised edges, clear boundaries of irregular shape. The site of inflammation is edematous, shiny, hot to the touch, painful on palpation. Sometimes bubbles, subcutaneous abscesses, and necrosis form on the surface of the focus.
Streptococcal toxic shock syndrome (STSS) is characterized by the acute development of shock and organ failure. The patient rapidly develops hypotensive shock with renal failure. Soft tissue infection is observed in 80% of patients and in most cases (70%) proceeds as severe subcutaneous infections (necrotizing fasciitis, myositis). Vesicles and bubbles on the surface of the inflammatory focus do not appear immediately and not in all patients and are an unfavorable prognostic sign. Mortality reaches 30%.
Early signs of STSS may include hyperemia of the conjunctiva and oropharyngeal mucosa, and a raspberry tongue.
Other cutaneous signs include petechial, maculopapular, and diffuse scarlet-like eruptions.
Acute diffuse streptoderma is characterized by the presence of flicten, prone to peripheral growth and fusion with the formation of large erosions, bordered by a corolla of the exfoliated epidermis. There is marked edema, hyperemia, profuse weeping, serous crusts. The process is localized, as a rule, on the lower extremities, as well as around infected wounds, fistulas, and burns.
Cellulite is an infectious inflammation of the dermis and subcutaneous fatty tissue. The inflammatory focus has a bright red color, indistinct contours, edematous, hot and painful on palpation. Vesicles, blisters, hemorrhages and even an abscess can be observed within the focus of inflammation. Cellulite can appear on any part of the skin, but more often it is localized on the skin of the lower extremities and face. Patients complain of malaise, body temperature rises.
Ecthyma vulgaris – deep tissue damage with ulceration in a limited area. The disease manifests itself with the appearance of bubbles with purulent contents, which for several days become covered with crusts, under which deep ulcers form. Scars form at the site of the ulcers.
Which doctors to contact
Consultation with a dermatologist, therapist or pediatrician is recommended if the patient is a child. Some patients require consultation with an endocrinologist.
Streptoderma treatment
The first rule of effective treatment is to protect streptoderma areas as much as possible from contact with water.
To dry the inflamed skin, the doctor prescribes treatment with a solution of brilliant green (brilliant green), fukarcin. An important stage of therapy is the use of external antibacterial drugs, and with a significant spread of the process, systemic antibiotics.
In the event of abscesses, boils, carbuncles https://en.wikipedia.org/wiki/Carbuncle, their surgical opening may be required.
With deep forms of streptoderma and chronic recurrent course of the disease, hormonal preparations and injections of staphylococcal toxoid are prescribed.
Complications
If, when the characteristic symptoms of streptoderma appear, the patient does not seek help on time, then the risk of complications increases:
if an infection enters the bloodstream, sepsis may develop;
non-healing ulcers – especially in patients with diabetes mellitus;
lesions of internal organs with staphylococcal infection;
intestinal dysbiosis;
fetal lesions during childbirth, if the mother has streptoderma areas on her body;
thrombophlebitis.
After severe streptoderma, scars may form on the skin.
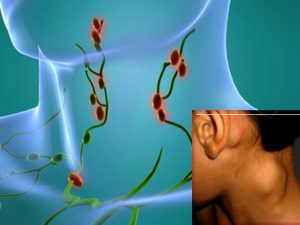
Complications of cellulite can be abscesses, osteomyelitis, septic arthritis, necrotizing fasciitis, as well as lymphangitis and glomerulonephritis. Recurrent lower extremity infections can be complicated by dermal fibrosis, lymph edema, and thickening of the epidermis.
Prevention of streptoderma
Preventive measures are aimed at early and active diagnosis, etiotropic treatment and isolation of patients in organized groups.
Personal prevention consists in observing hygiene standards, limiting contact with a patient with any streptococcal infection and timely treatment of any infectious pathologies.